1.3.12. More About Trace Minerals
Introduction
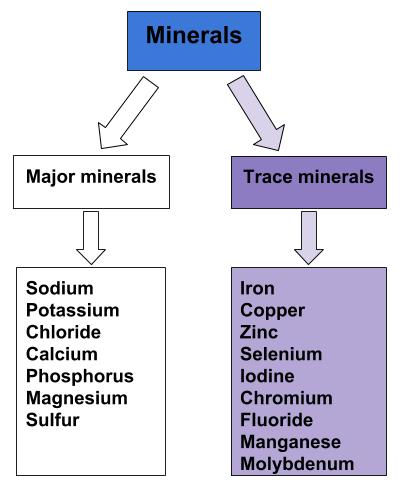
Trace minerals are classified as minerals required in the diet each day in smaller amounts, specifically 100 milligrams or less. These include copper, zinc, selenium, iodine, chromium, fluoride, manganese, molybdenum, and others. Although trace minerals are needed in smaller amounts it is important to remember that a deficiency in a trace mineral can be just as detrimental to your health as a major mineral deficiency. Iodine deficiency is a major concern in countries around the world.
Figure 1.3.12.1 The Trace Minerals
Iron
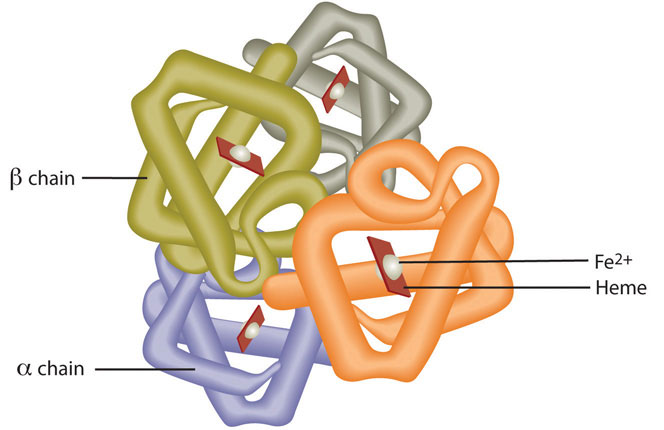
Red blood cells contain the oxygen-carrier protein hemoglobin. It is composed of four globular peptides, each containing a heme complex. In the center of each heme, lies iron (Figure 1.3.12.2 “The Structure of Hemoglobin”). Iron is needed for the production of other iron-containing proteins such as myoglobin. Myoglobin is a protein found in the muscle tissues that enhances the amount of available oxygen for muscle contraction. Iron is also a key component of hundreds of metabolic enzymes. Many of the proteins of the electron-transport chain contain iron–sulfur clusters involved in the transfer of high-energy electrons and ultimately ATP synthesis. Iron is also involved in numerous metabolic reactions that take place mainly in the liver and detoxify harmful substances. Moreover, iron is required for DNA synthesis. The great majority of iron used in the body is that recycled from the continuous breakdown of red blood cells.
Figure 1.3.12.2 The Structure of Hemoglobin
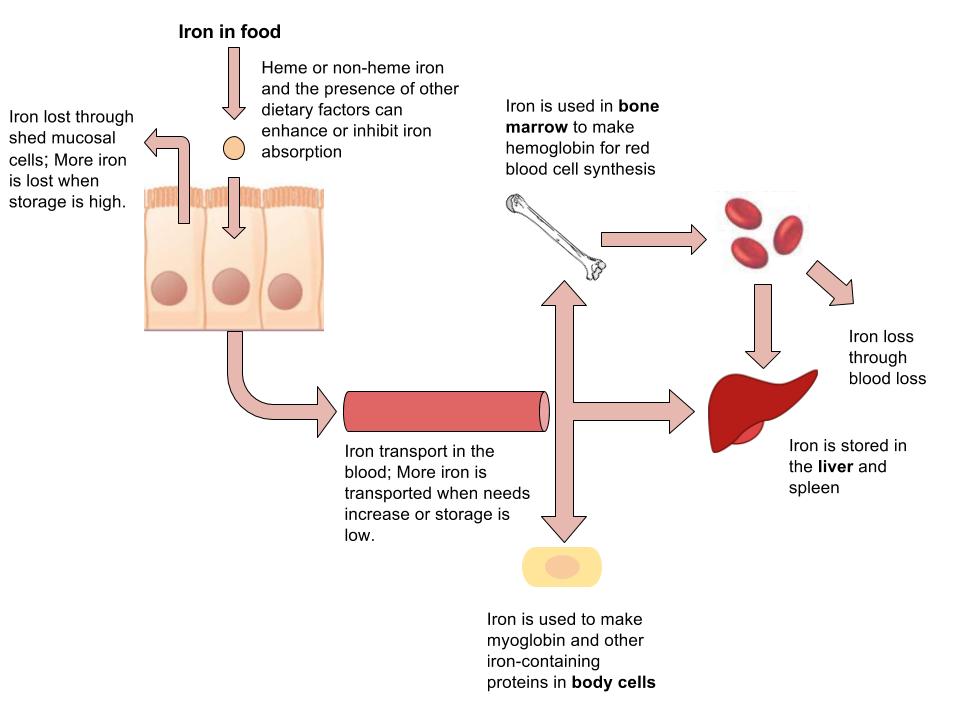
The iron in hemoglobin binds to oxygen in the capillaries of the lungs and transports it to cells where the oxygen is released. If iron level is low hemoglobin is not synthesized in sufficient amounts and the oxygen-carrying capacity of red blood cells is reduced, resulting in anemia. When iron levels are low in the diet the small intestine more efficiently absorbs iron in an attempt to compensate for the low dietary intake, but this process cannot make up for the excessive loss of iron that occurs with chronic blood loss or low intake. When blood cells are decommissioned for use, the body recycles the iron back to the bone marrow where red blood cells are made. The body stores some iron in the bone marrow, liver, spleen, and skeletal muscle. A relatively small amount of iron is excreted when cells lining the small intestine and skin cells die and in blood loss, such as during menstrual bleeding. The lost iron must be replaced from dietary sources.
The bioavailability of iron is highly dependent on dietary sources. In animal-based foods about 60 percent of iron is bound to hemoglobin, and heme iron is more bioavailable than nonheme iron. The other 40 percent of iron in animal-based foods is nonheme, which is the only iron source in plant-based foods. Some plants contain chemicals (such as phytate, oxalates, tannins, and polyphenols) that inhibit iron absorption. Although, eating fruits and vegetables rich in vitamin C at the same time as iron-containing foods markedly increases iron absorption. A review in the American Journal of Clinical Nutrition reports that in developed countries iron bioavailability from mixed diets ranges between 14 and 18 percent, and that from vegetarian diets ranges between 5 and 12 percent.[1] Vegans are at higher risk for iron deficiency, but careful meal planning does prevent its development. Iron deficiency is the most common of all micronutrient deficiencies.
Table 1.3.12.1 Enhancers and Inhibitors of Iron Absorption
| Enhancer | Inhibitor |
| Meat | Phosphate |
| Fish | Calcium |
| Poultry | Tea |
| Seafood | Coffee |
| Stomach acid | Colas |
| Soy protein | |
| High doses of minerals (antacids) | |
| Bran/fiber | |
| Phytates | |
| Oxalates | |
| Polyphenols |
Source: Iron.
Figure 1.3.12.3 Iron Absorption, Functions, and Loss
Iron Toxicity
The body excretes little iron and therefore the potential for accumulation in tissues and organs is considerable. Iron accumulation in certain tissues and organs can cause a host of health problems in children and adults including extreme fatigue, arthritis, joint pain, and severe liver and heart toxicity. In children, death has occurred from ingesting as little as 200 mg of iron and therefore it is critical to keep iron supplements out of children’s reach. Health Canada has set tolerable upper intake levels of iron at 40 for those under 14 years and 45 mg/day for those over the age of 14 years. Mostly a hereditary disease, hemochromatosis is the result of a genetic mutation that leads to abnormal iron metabolism and an accumulation of iron in certain tissues such as the liver, pancreas, and heart. The signs and symptoms of hemochromatosis are similar to those of iron overload in tissues caused by high dietary intake of iron or other non-genetic metabolic abnormalities, but are often increased in severity.
Dietary Sources of Iron
Table 1.3.12.2 Iron Content of Various Foods
| Food | Serving | Iron (mg) | Percent daily value |
| Breakfast cereals, fortified | 1 serving | 18 | 100 |
| Oysters | 3 oz. | 8 | 44 |
| Dark chocolate | 3 oz. | 7 | 39 |
| Beef liver | 3 oz. | 5 | 28 |
| Lentils | ½ c. | 3 | 17 |
| Spinach, boiled | ½ c. | 3 | 17 |
| Tofu, firm | ½ c. | 3 | 17 |
| Kidney beans | ½ c. | 2 | 11 |
| Sardines | 3 oz. | 2 | 11 |
Source: Iron.
Iron-Deficiency Anemia
Iron-deficiency anemia is a condition that develops from having insufficient iron levels in the body resulting in fewer and smaller red blood cells containing lower amounts of hemoglobin. Regardless of the cause (be it from low dietary intake of iron or via excessive blood loss), iron-deficiency anemia has the following signs and symptoms, which are linked to the essential functions of iron in energy metabolism and blood health:
- fatigue
- weakness
- pale skin
- shortness of breath
- dizziness
- swollen, sore tongue
- abnormal heart rate
Iron-deficiency anemia is diagnosed from characteristic signs and symptoms and confirmed with simple blood tests that count red blood cells and determine hemoglobin and iron content in blood. Anemia is most often treated with iron supplements and increasing the consumption of foods that are higher in iron. Iron supplements have some adverse side effects including nausea, constipation, diarrhea, vomiting, and abdominal pain. Reducing the dose at first and then gradually increasing to the full dose often minimizes the side effects of iron supplements. Avoiding foods and beverages high in phytates and also tea (which contains tannic acid and polyphenols, both of which impair iron absorption), is important for people who have iron-deficiency anemia. Eating a dietary source of vitamin C at the same time as iron-containing foods improves absorption of nonheme iron in the gut. Additionally, unknown compounds that likely reside in muscle tissue of meat, poultry, and fish increase iron absorption from both heme and nonheme sources. See Table 1.3.12.1 “Enhancers and Inhibitors of Iron Absorption” for more enhancers and inhibitors for iron absorption.
Iron Deficiency: A Worldwide Nutritional Health Problem
The Centers for Disease Control and Prevention reports that iron deficiency is the most common nutritional deficiency worldwide.[2] The main causes of iron deficiency worldwide are parasitic worm infections in the gut causing excessive blood loss, and malaria, a parasitic disease causing the destruction of red blood cells. In the developed world, iron deficiency is more the result of dietary insufficiency and/or excessive blood loss occurring during menstruation or childbirth.
At-Risk Populations
Infants, children, adolescents, and women are the populations most at risk worldwide for iron-deficiency anemia by all causes. Infants, children, and even teens require more iron because iron is essential for growth. In these populations, iron deficiency (and eventually iron-deficiency anemia) can also cause the following signs and symptoms: poor growth, failure to thrive, and poor performance in school, as well as mental, motor, and behavioral disorders. Women who experience heavy menstrual bleeding or who are pregnant require more iron in the diet. One more high-risk group is the elderly. Both elderly men and women have a high incidence of anemia and the most common causes are dietary iron deficiency and chronic disease such as ulcer, inflammatory diseases, and cancer. Additionally, those who have recently suffered from traumatic blood loss, frequently donate blood, or take excessive antacids for heartburn need more iron in the diet.
Preventing Iron-Deficiency Anemia
In young children iron-deficiency anemia can cause significant motor, mental, and behavioral abnormalities that are long-lasting. In the United States, the high incidence of iron-deficiency anemia in infants and children was a major public-health problem prior to the early 1970s, but now the incidence has been greatly reduced. This achievement was accomplished by implementing the screening of infants for iron-deficiency anemia in the health sector as a common practice, advocating the fortification of infant formulas and cereals with iron, and distributing them in supplemental food programs, such as that within Women, Infants, and Children (WIC). Breastfeeding, iron supplementation, and delaying the introduction of cow’s milk for at least the first twelve months of life were also encouraged. These practices were implemented across the socioeconomic spectrum and by the 1980s iron-deficiency anemia in infants had significantly declined. Other solutions had to be introduced in young children, who no longer were fed breast milk or fortified formulas and were consuming cow’s milk. The following solutions were introduced to parents: provide a diet rich in sources of iron and vitamin C, limit cow’s milk consumption to less than twenty-four ounces per day, and a multivitamin containing iron.
In the third world, iron-deficiency anemia remains a significant public-health challenge. The World Bank claims that a million deaths occur every year from anemia and that the majority of those occur in Africa and Southeast Asia. The World Bank states five key interventions to combat anemia:
- Provide at-risk groups with iron supplements.
- Fortify staple foods with iron and other micronutrients whose deficiencies are linked with anemia.
- Prevent the spread of malaria and treat the hundreds of millions with the disease.
- Provide insecticide-treated bed netting to prevent parasitic infections.
- Treat parasitic-worm infestations in high-risk populations.
Also, there is ongoing investigation as to whether supplying iron cookware to at-risk populations is effective in preventing and treating iron-deficiency anemia.
Copper
Copper, like iron, assists in electron transfer in the electron-transport chain. Furthermore, copper is a cofactor of enzymes essential for iron absorption and transport. The other important function of copper is as an antioxidant. Symptoms of mild to moderate copper deficiency are rare. More severe copper deficiency can cause anemia from the lack of iron mobilization in the body for red blood cell synthesis. Other signs and symptoms include growth retardation in children and neurological problems, because copper is a cofactor for an enzyme that synthesizes myelin, which surrounds many nerves.
Zinc
Zinc is a cofactor for over two hundred enzymes in the human body and plays a direct role in RNA, DNA, and protein synthesis. Zinc also is a cofactor for enzymes involved in energy metabolism. As the result of its prominent roles in anabolic and energy metabolism, a zinc deficiency in infants and children blunts growth. The reliance of growth on adequate dietary zinc was discovered in the early 1960s in the Middle East where adolescent nutritional dwarfism was linked to diets containing high amounts of phytate. Cereal grains and some vegetables contain chemicals, one being phytate, which blocks the absorption of zinc and other minerals in the gut. It is estimated that half of the world’s population has a zinc-deficient diet.[3]
This is largely a consequence of the lack of red meat and seafood in the diet and reliance on cereal grains as the main dietary staple. In adults, severe zinc deficiency can cause hair loss, diarrhea, skin sores, loss of appetite, and weight loss. Zinc is a required cofactor for an enzyme that synthesizes the heme portion of hemoglobin and severely deficient zinc diets can result in anemia.
Dietary Sources of Zinc
Table 1.3.12.3 Zinc Content of Various Foods
| Food | Serving | Zinc (mg) | Percent daily value |
| Oysters | 3 oz. | 74 | 493 |
| Beef, chuck roast | 3 oz. | 7 | 47 |
| Crab | 3 oz. | 6.5 | 43 |
| Lobster | 3 oz. | 3.4 | 23 |
| Pork loin | 3 oz. | 2.9 | 19 |
| Baked beans | ½ c. | 2.9 | 19 |
| Yogurt, low fat | 8 oz. | 1.7 | 11 |
| Oatmeal, instant | 1 packet | 1.1 | 7 |
| Almonds | 1 oz. | 0.9 | 6 |
Source: Fact Sheet for Health Professionals: Zinc. National Institute of Health, Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/. Updated February 11, 2016. Accessed November 10, 2017.
Selenium
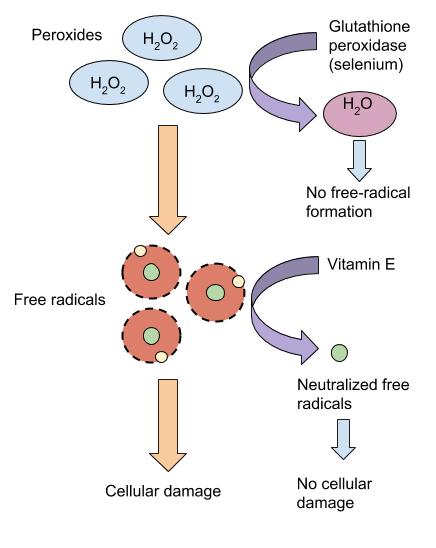
Selenium is a cofactor of enzymes that release active thyroid hormone in cells and therefore low levels can cause similar signs and symptoms as iodine deficiency. The other important function of selenium is as an antioxidant.
Selenium Functions and Health Benefits
Around twenty-five known proteins require selenium to function. Some are enzymes involved in detoxifying free radicals. Selenium also helps protect lipids from free radicals, and, in doing so, spares vitamin E. This is just one example of how antioxidants work together to protect the body against free-radical induced damage. Other functions of selenium-containing proteins include protecting endothelial cells that line tissues, converting the inactive thyroid hormone to the active form in cells, and mediating inflammatory and immune system responses.
Figure 1.3.12.4 Selenium’s Role in Detoxifying Free Radicals
Selenium at doses several thousand times the RDA can cause acute toxicity, and when ingested in gram quantities can be fatal. Chronic exposure to foods grown in soils containing high levels of selenium (significantly above the UL) can cause brittle hair and nails, gastrointestinal discomfort, skin rashes, halitosis, fatigue, and irritability.
Dietary Sources of Selenium
Organ meats, muscle meats, and seafood have the highest selenium content. Plants do not require selenium, so the selenium content in fruits and vegetables is usually low. Animals fed grains from selenium-rich soils do contain some selenium. Grains and some nuts contain selenium when grown in selenium-containing soils. See Table 1.3.12.4. “Selenium Contents of Various Foods” for the selenium content of various foods.
Table 1.3.12.4 Selenium Contents of Various Foods
| Food | Serving | Selenium (mcg) | Percent daily value |
| Brazil nuts | 1 oz. | 544 | 777 |
| Shrimp | 3 oz. | 34 | 49 |
| Crab meat | 3 oz. | 41 | 59 |
| Ricotta cheese | 1 c. | 41 | 59 |
| Salmon | 3 oz. | 40 | 57 |
| Pork | 3 oz. | 35 | 50 |
| Ground beef | 3 oz. | 18 | 26 |
| Round steak | 3 oz. | 28.5 | 41 |
| Beef liver | 3 oz. | 28 | 40 |
| Chicken | 3 oz. | 13 | 19 |
| Whole-wheat bread | 2 slices | 23 | 33 |
| Couscous | 1 c. | 43 | 61 |
| Barley, cooked | 1 c. | 13.5 | 19 |
| Milk, low-fat | 1 c. | 8 | 11 |
| Walnuts, black | 1 oz. | 5 | 7 |
Source: US Department of Agriculture, Agricultural Research Service. 2010. USDA National Nutrient Database for Standard Reference, Release 23. http://www.ars.usda.gov/ba/bhnrc/ndl. Updated December 10, 2019. Accessed October 24, 2020.
Iodine
Recall the discovery of iodine and its use as a means of preventing goiter, a gross enlargement of the thyroid gland in the neck. Iodine is essential for the synthesis of thyroid hormone, which regulates basal metabolism, growth, and development. Low iodine levels and consequently hypothyroidism has many signs and symptoms including fatigue, sensitivity to cold, constipation, weight gain, depression, and dry, itchy skin and paleness. The development of goiter may often be the most visible sign of chronic iodine deficiency, but the consequences of low levels of thyroid hormone can be severe during infancy, childhood, and adolescence as it affects all stages of growth and development. Thyroid hormone plays a major role in brain development and growth and fetuses and infants with severe iodine deficiency develop a condition known as cretinism, in which physical and neurological impairment can be severe. The World Health Organization (WHO) estimates iodine deficiency affects over two billion people worldwide and it is the number-one cause of preventable brain damage worldwide.[4]
Figure 1.3.12.5 Deaths Due to Iodine Deficiency Worldwide in 2012
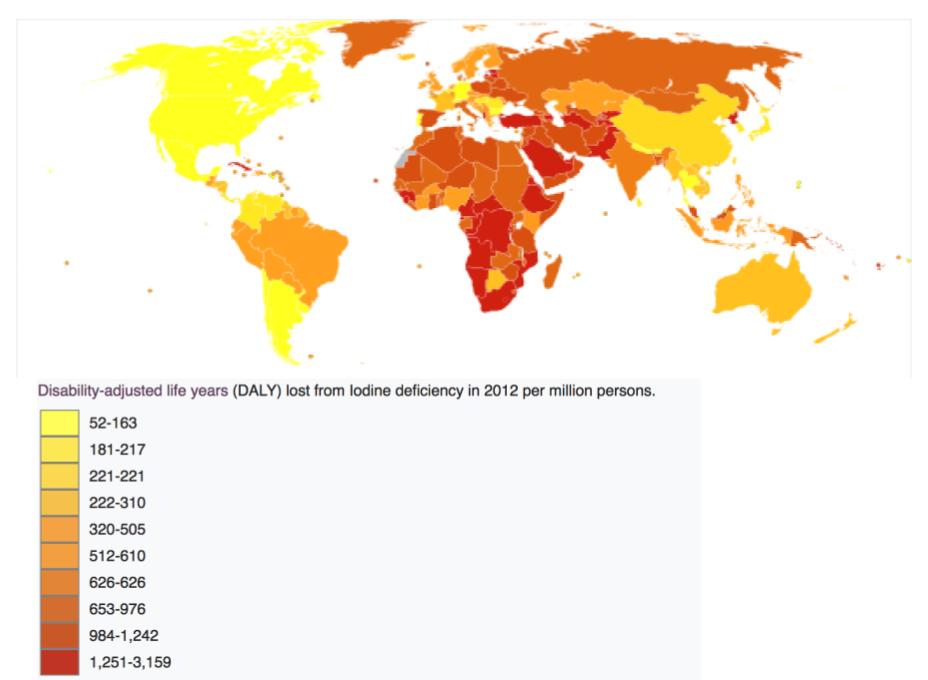
Figure 1.3.12.6 Iodine Deficiency: Goiter

Dietary Sources of Iodine
The mineral content of foods is greatly affected by the soil from which it grew, and thus geographic location is the primary determinant of the mineral content of foods. For instance, iodine comes mostly from seawater so the greater the distance from the sea the lesser the iodine content in the soil.
Table 1.3.12.5 Iodine Content of Various Foods
| Food | Serving | Iodine (mcg) | Percent daily value |
| Seaweed | 1 g. | 16 to 2,984 | 11 to 1,989 |
| Cod fish | 3 oz. | 99 | 66 |
| Yogurt, low fat | 8 oz. | 75 | 50 |
| Iodized salt | 1.5 g. | 71 | 47 |
| Milk, reduced fat | 8 oz. | 56 | 37 |
| Ice cream, chocolate | ½ c. | 30 | 20 |
| Egg | 1 large | 24 | 16 |
| Tuna, canned | 3 oz. | 17 | 11 |
| Prunes, dried | 5 prunes | 13 | 9 |
| Banana | 1 medium | 3 | 2 |
Source: Health Professional Fact Sheet: Iodine. National Institute of Health, Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/. Updated June 24, 2011. Accessed November 10, 2017.
Chromium
The functioning of chromium in the body is less understood than that of most other minerals. It enhances the actions of insulin so plays a role in carbohydrate, fat, and protein metabolism. More research is needed to better determine if chromium is helpful in treating certain chronic diseases and, if so, at what doses. Dietary sources of chromium include nuts, whole grains, and yeast.
Manganese
Manganese is a cofactor for enzymes that are required for carbohydrate and cholesterol metabolism, bone formation, and the synthesis of urea. Manganese deficiency is uncommon. The best food sources for manganese are whole grains, nuts, legumes, and green vegetables.
Molybdenum
Molybdenum also acts as a cofactor that is required for the metabolism of sulfur-containing amino acids, nitrogen-containing compounds found in DNA and RNA, and various other functions. The food sources of molybdenum is varies depending on the content in the soil in the specific region.
Fluoride
Fluoride’s Functional Role
Fluoride is known mostly as the mineral that combats tooth decay. It assists in tooth and bone development and maintenance. Fluoride combats tooth decay via three mechanisms:
- blocking acid formation by bacteria
- preventing demineralization of teeth
- enhancing remineralization of destroyed enamel
Fluoride was first added to drinking water in 1945 in Grand Rapids, Michigan; now over 60 percent of the US population consumes fluoridated drinking water. The Centers for Disease Control and Prevention (CDC) has reported that fluoridation of water prevents, on average, 27 percent of cavities in children and between 20 and 40 percent of cavities in adults. The CDC considers water fluoridation one of the ten great public health achievements in the twentieth century.[5]
Exposure to fluoride at three to five times this concentration before the growth of permanent teeth can cause fluorosis, which is the mottling and discoloring of the teeth.
Fluoride’s benefits to mineralized tissues of the teeth are well substantiated, but the effects of fluoride on bone are not as well known. In general, it appears that at low doses, fluoride treatment increases BMD in people with osteoporosis and is more effective in increasing bone quality when the intakes of calcium and vitamin D are adequate.
Dietary Sources of Fluoride
Table 1.3.12.6 Fluoride Content of Various Foods
| Food | Serving | Fluoride (mg) | Percent daily value* |
| Fruit Juice | 3.5 fl oz. | 0.02-2.1 | 0.7-70 |
| Crab, canned | 3.5 oz. | 0.21 | 7 |
| Rice, cooked | 3.5 oz. | 0.04 | 1.3 |
| Fish, cooked | 3.5 oz. | 0.02 | 0.7 |
| Chicken | 3.5 oz. | 0.015 | 0.5 |
| * Current AI used to determine Percent Daily Value |
Source: Micronutrient Information Center: Fluoride. Oregon State University, Linus Pauling Institute. lpi.oregonstate.edu/mic/minerals/fluoride . Updated in April 29, 2015. Accessed October 22, 2017.
- Centers for Disease Control and Prevention. “Iron and Iron Deficiency.” Accessed October 2, 2011. http://www.cdc.gov/nutrition/everyone/basics/vitamins/iron.html. ↵
- Iron and Iron Deficiency. Centers for Disease Control and Prevention. http://www.cdc.gov/nutrition/everyone/basics/vitamins/iron.html.Accessed October 2, 2011. ↵
- Prasad, A., “Zinc deficiency.” Br Med J. 2003 February 22; 326(7386): 409–10. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1125304/?tool=pmcentrez. Accessed October 2, 2011. ↵
- World Health Organization. “Iodine Status Worldwide.” http://whqlibdoc.who.int/publications/2004/9241592001.pdf. Accessed October 2, 2011. ↵
- 10 Great Public Health Achievements in the 20th Century. Centers for Disease Control, Morbidity and Mortality Weekly Report. 1999; 48(12), 241–43. http://www.cdc.gov/about/history/tengpha.htm. Accessed November 22, 2017. ↵

