1.3.11. More About Major Minerals
Introduction
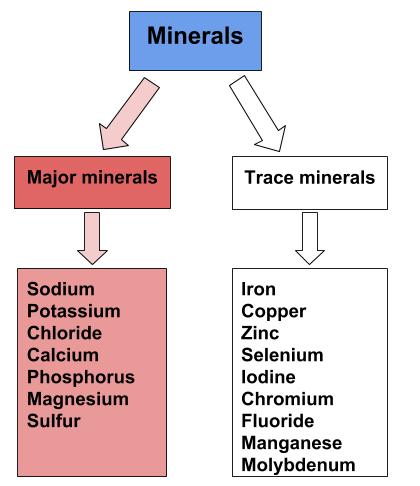
Similarly to vitamins, minerals are essential to human health and can be obtained in our diet from different types of food. Minerals are abundant in our everyday lives. From the soil in your front yard to the jewelry you wear on your body, we interact with minerals constantly. There are 20 essential minerals that must be consumed in our diets to remain healthy. The amount of each mineral found in our bodies vary greatly and therefore, so does consumption of those minerals. When there is a deficiency in an essential mineral, health problems may arise. Major minerals are classified as minerals that are required in the diet each day in amounts larger than 100 milligrams. These include sodium, potassium, chloride, calcium, phosphorus, magnesium, and sulfur. These major minerals can be found in various foods. Consuming a varied diet significantly improves an individual’s ability to meet their nutrient needs. [1]
Figure 1.3.11.1 The Major Minerals
Bioavailability
Minerals are not as efficiently absorbed as most vitamins and so the bioavailability of minerals can be very low. Plant-based foods often contain factors, that bind to minerals and inhibit their absorption. In general, minerals are better absorbed from animal-based foods. In most cases, if dietary intake of a particular mineral is increased, absorption will decrease. Some minerals influence the absorption of others. For instance, excess zinc in the diet can impair iron and copper absorption. Conversely, certain vitamins enhance mineral absorption. For example, vitamin C boosts iron absorption, and vitamin D boosts calcium and magnesium absorption. As is the case with vitamins, certain gastrointestinal disorders and diseases, such as Crohn’s disease and kidney disease, as well as the aging process, impair mineral absorption, putting people with malabsorption conditions and the elderly at higher risk for mineral deficiencies.
Calcium
Calcium’s Functional Roles
Calcium is the most abundant mineral in the body and greater than 99 percent of it is stored in bone tissue. Although only 1 percent of the calcium in the human body is found in the blood and soft tissues, it is here that it performs the most critical functions. Blood calcium levels are rigorously controlled so that if blood levels drop the body will rapidly respond by stimulating bone resorption, thereby releasing stored calcium into the blood. Thus, bone tissue sacrifices its stored calcium to maintain blood calcium levels. This is why bone health is dependent on the intake of dietary calcium and also why blood levels of calcium do not always correspond to dietary intake.
Calcium plays a role in a number of different functions in the body like bone and tooth formation. The most well-known calcium function is to build and strengthen bones and teeth.
When your diet is calcium deficient, the mineral content of bone decreases causing it to become brittle and weak. Thus, increased calcium intake helps to increase the mineralized content of bone tissue. Greater mineralized bone tissue corresponds to a greater BMD, and to greater bone strength. The remaining calcium plays a role in nerve impulse transmission by facilitating electrical impulse transmission from one nerve cell to another. Calcium in muscle cells is essential for muscle contraction because the flow of calcium ions are needed for the muscle proteins (actin and myosin) to interact. Calcium is also essential in blood clotting by activating clotting factors to fix damaged tissue.
In addition to calcium’s four primary functions calcium has several other minor functions that are also critical for maintaining normal physiology. For example, without calcium, the hormone insulin could not be released from cells in the pancreas and glycogen could not be broken down in muscle cells and used to provide energy for muscle contraction.
Figure 1.3.11.2 Maintaining Blood Calcium Levels

Other Health Benefits of Calcium in the Body
Besides forming and maintaining strong bones and teeth, calcium has been shown to affect other aspects of health, including:
- cancer: The National Cancer Institute reports that there is enough scientific evidence to conclude that higher intakes of calcium decrease colon cancer risk and may suppress the growth of polyps that often precipitate cancer. Although higher calcium consumption protects against colon cancer, some studies have looked at the relationship between calcium and prostate cancer and found higher intakes may increase the risk for prostate cancer; however the data is inconsistent and more studies are needed to confirm any negative association.
- blood pressure: Multiple studies provide clear evidence that higher calcium consumption reduces blood pressure. A review of twenty-three observational studies concluded that for every 100 milligrams of calcium consumed daily, systolic blood pressure is reduced 0.34 millimeters of mercury (mmHg) and diastolic blood pressure is decreased by 0.15 mmHg.[1]
- cardiovascular health: There is emerging evidence that higher calcium intakes prevent against other risk factors for cardiovascular disease, such as high cholesterol and obesity, but the scientific evidence is weak or inconclusive.
- kidney stones: Another health benefit of a high-calcium diet is that it blocks kidney stone formation. Calcium inhibits the absorption of oxalate, a chemical in plants such as parsley and spinach, which is associated with an increased risk for developing kidney stones. Calcium’s protective effects on kidney stone formation occur only when you obtain calcium from dietary sources. Calcium supplements may actually increase the risk for kidney stones in susceptible people.
Figure 1.3.11.3 Calcium’s Effect on Aging
Despite the wealth of evidence supporting the many health benefits of calcium (particularly bone health), the average North American diet falls short of achieving the recommended dietary intakes of calcium. In fact, in females older than nine years of age, the average daily intake of calcium is only about 70 percent of the recommended intake. Here we will take a closer look at particular groups of people who may require extra calcium intake:
- adolescent teens: A calcium-deficient diet is common in teenage girls as their dairy consumption often considerably drops during adolescence.
- amenorrheic women and the “female athlete triad”: Amenorrhea refers to the absence of a menstrual cycle. Women who fail to menstruate suffer from reduced estrogen levels, which can disrupt and have a negative impact on the calcium balance in their bodies. The “female athlete triad” is a combination of three conditions characterized by amenorrhea, disrupted eating patterns, and osteoporosis. Exercise-induced amenorrhea and anorexia nervosa-related amenorrhea can decrease bone mass.[2] In female athletes, as well as active women in the military, low BMD, menstrual irregularities, and individual dietary habits together with a history of previous stress issues are related to an increased susceptibility to future stress fractures.[3]
- elderly people: As people age, calcium bioavailability is reduced, the kidneys lose their capacity to convert vitamin D to its most active form, the kidneys are no longer efficient in retaining calcium, the skin is less effective at synthesizing vitamin D, there are changes in overall dietary patterns, and older people tend to get less exposure to sunlight. Thus the risk for calcium inadequacy is great.[4]
- postmenopausal women: Estrogen enhances calcium absorption. The decline in this hormone during and after menopause puts postmenopausal women especially at risk for calcium deficiency. Decreases in estrogen production are responsible for an increase in bone resorption and a decrease in calcium absorption. During the first years of menopause, annual decreases in bone mass range from 3–5 percent. After age sixty-five, decreases are typically less than 1 percent.[5]
- lactose-intolerant people: Groups of people, such as those who are lactose intolerant, or who adhere to diets that avoid dairy products, may not have an adequate calcium intake.
- vegans: Vegans typically absorb reduced amounts of calcium because their diets favour plant-based foods that contain oxalates and phytates. [6]In addition, because vegans avoid dairy products, their overall consumption of calcium-rich foods may be less.
If you are lactose intolerant, have a milk allergy, are a vegan, or you simply do not like dairy products, remember that there are many plant-based foods that have a good amount of calcium and there are also some low-lactose and lactose-free dairy products on the market.
Diet, Supplements, and Chelated Supplements
In general, calcium supplements perform to a lesser degree than dietary sources of calcium in providing many of the health benefits linked to higher calcium intake. This is partly attributed to the fact that dietary sources of calcium supply additional nutrients with health-promoting activities.
Vitamin D has to be activated and in the bloodstream to promote calcium absorption. Thus, it is important to maintain an adequate intake of vitamin D.
Dietary Sources of Calcium
In the typical North American diet, calcium is obtained mostly from dairy products, primarily cheese. A slice of cheddar or Swiss cheese contains just over 200 milligrams of calcium. One cup of nonfat milk contains approximately 300 milligrams of calcium, which is about a third of the RDA for calcium for most adults. Foods fortified with calcium such as cereals, soy milk, and orange juice also provide one third or greater of the calcium RDA. Although the typical American diet relies mostly on dairy products for obtaining calcium, there are other good non-dairy sources of calcium.
Tools for Change
If you need to increase calcium intake, are a vegan, or have a food allergy to dairy products, it is helpful to know that there are some plant-based foods that are high in calcium. Tofu (made with calcium sulfate), turnip greens, mustard greens, and Chinese cabbage are good sources. For a list of non-dairy sources you can find the calcium content for thousands of foods by visiting the USDA National Nutrient Database (http://www.nal.usda.gov/fnic/foodcomp/search/). When obtaining your calcium from a vegan diet, it is important to know that some plant-based foods significantly impair the absorption of calcium. These include spinach, Swiss chard, rhubarb, beets, cashews, and peanuts. With careful planning and good selections, you can ensure that you are getting enough calcium in your diet even if you do not drink milk or consume other dairy products.
Table 1.3.11.1 Calcium Content of Various Foods
| Food | Serving | Calcium (mg) | Percent Daily Value |
| Yogurt, low fat | 8 oz. | 415 | 42 |
| Mozzarella | 1.5 oz. | 333 | 33 |
| Sardines, canned with bones | 3 oz. | 325 | 33 |
| Cheddar Cheese | 1.5 oz. | 307 | 31 |
| Milk, nonfat | 8 oz. | 299 | 30 |
| Soymilk, calcium fortified | 8 oz. | 299 | 30 |
| Orange juice, calcium fortified | 6 oz. | 261 | 26 |
| Tofu, firm, made with calcium sulfate | ½ c. | 253 | 25 |
| Salmon, canned with bones | 3 oz. | 181 | 18 |
| Turnip, boiled | ½ c. | 99 | 10 |
| Kale, cooked | 1 c. | 94 | 9 |
| Vanilla Ice Cream | ½ c. | 84 | 8 |
| White bread | 1 slice | 73 | 7 |
| Kale, raw | 1 c. | 24 | 2 |
| Broccoli, raw | ½ c. | 21 | 2 |
Source: Fact Sheet for Health Professionals: Calcium. National Institute of Health, Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/. Updated November 17, 2016. Accessed November 12, 2017.
Calcium Bioavailability
In the small intestine, calcium absorption primarily takes place in the duodenum (first section of the small intestine) when intakes are low, but calcium is also absorbed passively in the jejunum and ileum (second and third sections of the small intestine), especially when intakes are higher. The body doesn’t completely absorb all the calcium in food. Interestingly, the calcium in some vegetables such as kale, brussel sprouts, and bok choy is better absorbed by the body than are dairy products. About 30 percent of calcium is absorbed from milk and other dairy products.
The greatest positive influence on calcium absorption comes from having an adequate intake of vitamin D. People deficient in vitamin D absorb less than 15 percent of calcium from the foods they eat. The hormone estrogen is another factor that enhances calcium bioavailability. Thus, as a woman ages and goes through menopause, during which estrogen levels fall, the amount of calcium absorbed decreases and the risk for bone disease increases. Some fibers, such as inulin, found in jicama, onions, and garlic, also promote calcium intestinal uptake.
Chemicals that bind to calcium decrease its bioavailability. These negative effectors of calcium absorption include the oxalates in certain plants, the tannins in tea, phytates in nuts, seeds, and grains, and some fibers. Oxalates are found in high concentrations in spinach, parsley, cocoa, and beets. In general, the calcium bioavailability is inversely correlated to the oxalate content in foods. High-fiber, low-fat diets also decrease the amount of calcium absorbed, an effect likely related to how fiber and fat influence the amount of time food stays in the gut. Anything that causes diarrhea, including sickness, medications, and certain symptoms related to old age, decreases the transit time of calcium in the gut and therefore decreases calcium absorption. As we get older, stomach acidity sometimes decreases, diarrhea occurs more often, kidney function is impaired, and vitamin D absorption and activation is compromised, all of which contribute to a decrease in calcium bioavailability.
Phosphorus
Phosphorus is present in our bodies as part of a chemical group called a phosphate group. These phosphate groups are essential as a structural component of cell membranes (as phospholipids), DNA and RNA, energy production (ATP), and regulation of acid-base homeostasis. Phosphorus however is mostly associated with calcium as a part of the mineral structure of bones and teeth. Blood phosphorus levels are not controlled as strictly as calcium so the PTH stimulates renal excretion of phosphate so that it does not accumulate to toxic levels.
In comparison to calcium, most Americans are not at risk for having a phosphate deficiency. Phosphate is present in many foods popular in the American diet including meat, fish, dairy products, processed foods, and beverages. Phosphate is added to many foods because it acts as an emulsifying agent, prevents clumping, improves texture and taste, and extends shelf-life.
Dietary Sources of Phosphorus
Table 1.3.11.2 Phosphorus Content of Various Foods
| Foods | Serving | Phosphorus (mg) | Percent Daily Value 1000 |
| Salmon | 3 oz. | 315 | 32 |
| Yogurt, nonfat | 8 oz. | 306 | 31 |
| Turkey, light meat | 3 oz. | 217 | 22 |
| Chicken, light meat | 3 oz. | 135 | 14 |
| Beef | 3 oz. | 179 | 18 |
| Lentils* | ½ c. | 178 | 18 |
| Almonds* | 1 oz. | 136 | 14 |
| Mozzarella | 1 oz. | 131 | 13 |
| Peanuts* | 1 oz. | 108 | 11 |
| Whole wheat bread | 1 slice | 68 | 7 |
| Egg | 1 large | 86 | 9 |
| Carbonated cola drink | 12 oz. | 41 | 4 |
| Bread, enriched | 1 slice | 25 | 3 |
Source: Micronutrient Information Center: Phosphorus. Oregon State University, Linus Pauling Institute. http://lpi.oregonstate.edu/mic/minerals/phosphorus. Updated in July 2013. Accessed October 22, 2017.
Sulphur
Sulphur’s Functions in the Body
Sulphur is the third most abundant mineral in the body, after calcium and phosphorus. Sulphur is incorporated into protein structures in the body. Amino acids, methionine and cysteine contain sulfur which are essential for the antioxidant enzyme glutathione peroxidase. Some vitamins like thiamin and biotin also contain sulphur which are important in regulating acidity in the body. Sulphur is additional essential for insulin production, which regulates blood glucose levels.
Sulphur is a major mineral with no recommended intake or deficiencies when protein needs are met.
Dietary Sources of Sulphur
Sulfur is mostly consumed as a part of dietary proteins and sulfur containing vitamins. Sulphur can be found in diary, meats, onions, garlic, and kale.
Table 1.3.11.3 Sulphur Content of Various Foods
| Food | Serving | Sulphur (mg) |
| White bread | 25g | 80 |
| Spagetti noodles | 120g | 30 |
| Rice | 160g | 30 |
| Egg, boiled | 55g | 180 |
| Butter, salted | 10g | – |
| Haddock | 100g | 290 |
| Tuna, canned | 120g | – |
| Apricots, dried | 25g | 160 |
| Chicken | 100g | 300 |
| Cheddar | 25g | 230 |
| Onions | ¼=20g | 50 |
| Spinach, boiled | 60g | 90 |
Source: Elements – 31: Sulphur. National Human Rights Institutions. http://apjcn.nhri.org.tw/server/info/books-phds/books/foodfacts/html/data/data5g.html. Accessed Jan 1, 2020.
Magnesium
Magnesium’s Functional Role
In addition to participating in bone maintenance, magnesium has several other functions in the body. In every reaction involving the cellular energy molecule, ATP, magnesium is required. More than three hundred enzymatic reactions require magnesium. Magnesium plays a role in the synthesis of DNA and RNA, carbohydrates, and lipids, and is essential for nerve conduction and muscle contraction. Another health benefit of magnesium is that it may decrease blood pressure.
Many Americans do not get the recommended intake of magnesium from their diets. Some observational studies suggest mild magnesium deficiency is linked to increased risk for cardiovascular disease. Signs and symptoms of severe magnesium deficiency may include tremor, muscle spasms, loss of appetite, and nausea.
Dietary Sources of Magnesium
Magnesium is part of the green pigment, chlorophyll, which is vital for photosynthesis in plants; therefore green leafy vegetables are a good dietary source for magnesium. Magnesium is also found in high concentrations in fish, dairy products, meats, whole grains, and nuts. Additionally chocolate, coffee, and hard water contain a good amount of magnesium. Most people in America do not fulfill the RDA for magnesium in their diets. Typically, Western diets lean toward a low fish intake and the unbalanced consumption of refined grains versus whole grains.
Table 1.3.11.4 Magnesium Content of Various Foods
| Food | Serving | Magnesium (mg) | Percent daily value |
| Almonds | 1 oz. | 80 | 20 |
| Cashews | 1 oz. | 74 | 19 |
| Soymilk | 1 c. | 61 | 15 |
| Black beans | ½ c. | 60 | 15 |
| Edamame | ½ c. | 50 | 13 |
| Bread | 2 slices | 46 | 12 |
| Avocado | 1 c. | 44 | 11 |
| Brown rice | ½ c. | 42 | 11 |
| Yogurt | 8 oz. | 42 | 11 |
| Oatmeal, instant | 1 packet | 36 | 9 |
| Salmon | 3 oz. | 26 | 7 |
| Chicken breasts | 3 oz. | 22 | 6 |
| Apple | 1 medium | 9 | 2 |
Source: Dietary Supplement Fact Sheet: Magnesium. National Institutes of Health, Office of Dietary Supplements. http://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/. Updated July 13, 2009. Accessed November 12, 2017.
Sodium
Sodium’s Functional Role
Sodium is an essential nutrient found in salt and many foods. In the body sodium functions to maintain the balance of water in cells, allows for proper muscle and nerve function and helps to maintain a stable blood pressure. Although a small amount of sodium is necessary for health, too much sodium can lead to numerous health conditions such as high blood pressure, stroke, heart disease and kidney disease. High sodium intake has also been linked to an increased risk for osteoporosis, stomach cancer and asthma. [7]
The recommended dietary intake of sodium in Canada is between 1000-1500 mg per day. People who are 14 years or older should not consume more than 2300 mg of sodium per day as consumption this high increases the risk of an adverse health event. [8]
Dietary Sources of Sodium
The average Canadian eats 3400mg of sodium each day, more than double the amount needed. Sodium is added to many foods to add flavor and is used as a preservative. Most of the sodium we eat comes from processed and pre-packaged foods. Deli meat, frozen pizzas and fast foods are examples of these foods. The second highest dietary source of sodium comes from naturally occurring sources such as milk, fresh meat and fruits and vegetables. The third highest dietary source of sodium is the in the products we add during cooking. These include sauces, pre-mixed spices and condiments. Lastly, the salt we add at the table makes up the smallest source of dietary sodium that we consume. [9]
Follow this link to see a detailed break down of the leading dietary sources of sodium in Canada.
Table 1.3.11.5 Sodium Content of Various Foods
| Food | Serving | Sodium (mg) | Percent daily value |
| Salted nuts | 100g | 780 | 52 |
| Tuna | 100g | 310 | 20 |
| Canned tomatoes | 100g | 420 | 28 |
| Chicken soup | 100g | 385 | 26 |
| Table salt | 1 tsp | 2300 | 153 |
| Soy sauce | 1 tsp | 1032 | 69 |
| Sausage | 100g | 1235 | 82 |
| Smoked salmon | 100g | 784 | 52 |
| Hamburger | 100g | 561 | 37 |
| Cheddar cheese | 100g | 620 | 41 |
| Mozzarella | 100g | 373 | 25 |
| Butter | 100g | 286 | 19 |
| Corn flakes | 100 | 900 | 60 |
Source: Sodium Content Chart. https://i.pinimg.com/736x/7e/5f/2a/7e5f2a60ec28602951f07470ea14359f–at-the-table-charts.jpg Accessed January 1, 2020.
Salt Sensitivity
High dietary intake of sodium is one risk factor for hypertension and contributes to high blood pressure in many people. However, studies have shown that not everyone’s blood pressure is affected by lowering sodium intake. About 10 to 20 percent of the population is considered to be salt-sensitive, meaning their blood pressure is affected by salt intake. Genetics, race, gender, weight, and physical activity level are determinants of salt sensitivity. African Americans, women, and overweight individuals are more salt-sensitive than others. Also, if hypertension runs in a person’s family, that person is more likely to be salt-sensitive.
The Benefits of Sodium Reduction
In Canada it has been estimated that if the average sodium intake was reduced by 1840 mg per day there would be a 30% decrease in the prevalence of high blood pressure. [10]
Everyone can benefit from eating less sodium. When choosing foods remember that a sodium content of 5% or less is a little sodium and 15% or more is a lot of sodium. When at the grocery store avoid processed, pre-packaged foods. Always check the sodium content to ensure you are not purchasing a product that contains high amounts of hidden sodium. Additionally, add flavor to foods with herds, whole spices or lemon juice instead of salt. [11]
Potassium
Potassium’s Functional Roles
Potassium is an essential mineral found in many foods. Potassium is involved in many of the same functions as sodium. Potassium helps to regulate fluid balance, muscle contractions and nerve signals. Contrary to sodium, a high potassium diet may help reduce blood pressure and protect against stroke, osteoporosis and kidney disease. Whereas a low potassium intake has been associated with hypertension and several chronic diseases [12]
Dietary Sources of Potassium
Potassium can be found in a variety of foods. Foods containing high sources of potassium include bananas, apricots, kiwifruit, milk and yogurt, salmon and cooked vegetables such as broccoli, spinach and potatoes.[13] Most Canadians will get enough potassium as long as they are eating a well balanced diet. However, in several developed countries, including Canada, diets are high in processed foods and low in fresh fruits and vegetables leading to a potassium consumption that is too low compared to sodium consumption.
In Canada it is recommended that individuals over the age of 14 consume 4700 mg of potassium per day. The healthy individual can obtain their required potassium intake through a proper diet. Potassium supplements should not be used unless a doctor has recommended them.
Potassium salt (potassium chloride) can be used as an alternative to salt both at the table and in the making of processed foods to reduce sodium content without sacrificing flavor. Health Canada is in the processed of approving several potassium additives to replace sodium additives in the making of processed and preserved foods. [14]
Vegetables and fruits are the best sources of potassium. Grains, dairy, lentils and meat also contain potassium. The table below details a variety of foods and their potassium contents.
Table 1.3.11.6 Potassium Content of Various Foods
| Food | Serving | Potassium (mg) | Percent daily value |
| Tomato paste | 60 mL (¼ cup) | 658 | 14 |
| Potato, baked | 1 (12cm x 6cm) | 610 | 13 |
| Pinto or kidney beans | 175 mL (3/4 cup) | 566 to 591 | 13 |
| Lentils | 175 mL (3/4 cup) | 579 | 12 |
| Avocado | ½ whole | 487 | 10 |
| Squash, baked | 125 mL (1/2 cup) | 473 | 10 |
| Banana | 1 medium | 422 | 9 |
| Papaya | ½ medium | 392 | 8 |
| Milk, 2% | 250 mL (1 cup) | 387 | 8 |
| Chickpeas | 175 mL (3/4 cup) | 378 | 8 |
| Yogurt | 175 g (3/4 cup) | 362 | 8 |
| Fish | 75 g (2 ½ oz) | 313 | 7 |
Source: What you need to know about potassium. Unlock food. https://www.unlockfood.ca/en/Articles/Vitamins-and-Minerals/What-You-Need-to-Know-About-Potassium.aspx]. Updated March 21, 2019. Accessed January 1, 2020.
Chloride
Chloride’s Functional Roles
Chloride’s main function in the body is to maintain fluid balance. It also helps to maintain blood volume, blood pressure and the pH of body fluids. Chloride toxicity is rarely observed in humans, except in some diseased states. A healthy individual can tolerate high quantities of chloride as long as there is a source of clean drinking water.
Dietary Sources of Chloride
Chloride is consumed as sodium chloride (NaCl) and potassium chloride (KCl) salts which are widely distributed in a variety of food sources. Table salt is mainly composed of sodium chloride, therefore a diet that contains salt with also contain chloride. Chloride is also found in drinking water as a results of natural salt depositions in the earth. Data from several of Canada’s provinces indicates that chloride’s content in drinking water is often relatively low at 10mg/L. [15]
- Pobocik RS, Trager A, Monson LM. Dietary Patterns and Food Choices of a Population Sample of Adults on Guam. Asia Pacific Journal of Clinical Nutrition. 2008; 17(1), 94-100. http://apjcn.nhri.org.tw/server/APJCN/17/1/94.pdf. Accessed February 16, 2018. ↵
- Drinkwater B, Bruemner B, Chesnut C. Menstrual History As a Determinant of Current Bone Density in Young Athletes. JAMA. 1990; 263(4), 545–8. http://www.ncbi.nlm.nih.gov/pubmed/2294327?dopt=Abstract. . Accessed November 22, 2017. ↵
- Nattiv A. Stress Fractures and Bone Health in Track and Field Athletes. J Sci Med Sport. 2000; 3(3), 268–79. http://www.ncbi.nlm.nih.gov/pubmed/11101266?dopt=Abstract. Accessed November 22, 2017. ↵
- Calcium and Vitamin D in the Elderly. International Osteoporosis Foundation. http://www.iofbonehealth.org/patients-public/about-osteoporosis/prevention/nutrition/calcium-and-vitamin-d-in-the-elderly.html. Published 2012. Accessed November 22, 2017. ↵
- Daniels CE. Estrogen Therapy for Osteoporosis Prevention in Postmenopausal Women. National Institute of Health: Pharmacy. Update March/April 2000. ↵
- Ross. C., et al. Dietary Reference Intakes for Calcium and Vitamin D.Food and Nutrition Board, Institute of Medicine. Washington, DC: National Academy Press. 2010. https://pubmed.ncbi.nlm.nih.gov/21796828/. Accessed Nov 14, 2020. ↵
- Sodium in Canada. Health Canada. https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium.html. Updated March 1, 2017. Accessed January 1, 2020. ↵
- Sodium in Canada. Health Canada. https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium.html. Updated March 1, 2017. Accessed January 1, 2020. ↵
- Sodium Detector. Health Canada. https://health.canada.ca/en/health-canada/services/food-nutrition/food-guides-healthy-eating/nutrients/sodium/detector.html. Updated January 16, 2018. Accessed January 1, 2020. ↵
- Sodium in Canada. Health Canada. https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium.html. Updated March 1, 2017. Accessed January 1, 2020. ↵
- About Sodium. Health Canada. https://www.canada.ca/en/health-canada/services/nutrients/sodium/sodium.html. Updated January 12, 2012. Accessed January 1, 2020. ↵
- Dietary Potassium. Hypertension Canada. https://hypertension.ca/wp-content/uploads/2019/01/Position-Statement-on-Dietary-Potassium-Hypertension-Canada-January-2019.pdf. Updated January 2019. Accessed January 1, 2020. ↵
- Dietary Potassium. Hypertension Canada. https://hypertension.ca/wp-content/uploads/2019/01/Position-Statement-on-Dietary-Potassium-Hypertension-Canada-January-2019.pdf. Updated January 2019. Accessed January 1, 2020. ↵
- Health Canada's Proposal to Enable the Use of Potassium Acetate and Potassium Diacetate as Preservatives in Meat and Poultry Products. Health Canada. https://www.canada.ca/en/health-canada/services/food-nutrition/public-involvement-partnerships/proposal-use-potassium-acetate-potassium-diacetate-preservatives-meat-poultry-products/consultation.html. Updated June 7, 2016. Accessed January 1, 2020. ↵
- Guidelines for Canadian Drinking Water Quality. Health Canada. https://www.canada.ca/en/health-canada/services/publications/healthy-living/guidelines-canadian-drinking-water-quality-guideline-technical-document-chloride.html. Updated January 7, 2008. Accessed January 1, 2020. ↵

