Mood Disorders
Leanne Stevens; Jennifer Stamp; Kevin LeBlanc (editors - original chapter); and Jessica Motherwell McFarlane (editor - adapted chapter)
Blake cries all day, feels worthless and believes that life is hopeless; he cannot get out of bed. Keisha stays up all night and talks very rapidly; she went on a shopping spree in which she spent $3,000 on furniture, although she cannot afford it. Skylar recently had a baby; they feel overwhelmed, teary, anxious, and panicked practically every day since the baby was born. Skylar also believes they are a terrible parent. All these individuals demonstrate symptoms of a potential mood disorder.
Mood disorders (Figure PD.14) are characterised by severe disturbances in mood and emotions — most often depression, but also mania and elation (Rothschild, 1999). All of us experience fluctuations in our moods and emotional states, and often these fluctuations are caused by events in our lives. We become elated if our favourite team wins the World Series and dejected if a romantic relationship ends or if we lose our job. At times, we feel fantastic or miserable for no clear reason. People with mood disorders also experience mood fluctuations, but their fluctuations are extreme, distort their outlook on life, and impair their ability to function.

The DSM-5 lists two general categories of mood disorders. Bipolar and related disorders are a group of disorders in which mania is the defining feature. Mania is a state of extreme elation, agitation, heightened energy, reduced need for sleep, grandiosity, impulsive behaviour, and rapid speech. When people experience mania, they may become extremely talkative, behave recklessly, or attempt to take on many tasks simultaneously. The most recognised of these disorders is bipolar disorder.
Depressive disorders are a group of disorders in which depression is the main feature. Depression is a vague term that, in everyday language, refers to an intense and persistent sadness and feelings of disconnection. Depression is a diverse and varied mood state — it consists of a broad spectrum of symptoms that range in severity. Depressed people feel sad, discouraged and hopeless. These individuals lose interest in activities once enjoyed, often experience a decrease in drives such as hunger and sex, and frequently doubt personal worth.
Depressive disorders vary by degree, but this chapter highlights the most well-known: major depressive disorder (sometimes called unipolar depression).
Major Depressive Disorder
According to the DSM-5, the defining symptoms of major depressive disorder include “depressed mood most of the day, nearly every day” (feeling sad, empty, hopeless, or appearing tearful to others), and loss of interest and pleasure in usual activities (APA, 2013). In addition to feeling overwhelmingly sad most of each day, people with depression will no longer show interest or enjoyment in activities that previously were gratifying, such as hobbies, sports, sex, social events, time spent with family, and so on. Friends and family members may notice that the person has completely abandoned previously enjoyed hobbies; for example, an avid tennis player who develops major depressive disorder no longer plays tennis (Rothschild, 1999).
To receive a diagnosis of major depressive disorder, one must experience a total of five symptoms for at least a two-week period; these symptoms must cause significant distress or impair normal functioning, and they must not be caused by substances or a medical condition. At least one of the two symptoms mentioned above must be present, plus any combination of the following symptoms (APA, 2013):
- significant weight loss (when not dieting) or weight gain and/or significant decrease or increase in appetite;
- difficulty falling asleep or sleeping too much;
- psychomotor agitation (the person is noticeably fidgety and jittery, demonstrated by behaviours like the inability to sit, pacing, handwringing, and pulling or rubbing of the skin, clothing, or other objects) or psychomotor retardation (the person talks and moves slowly, for example, talking softly, very little, or in a monotone);
- fatigue or loss of energy;
- feelings of worthlessness or guilt;
- difficulty concentrating and indecisiveness; and
- suicidal ideation: thoughts of death (not just fear of dying), thinking about or planning suicide, or making an actual suicide attempt.
Major depressive disorder is considered episodic; its symptoms are typically present at their full magnitude for a certain period of time and then gradually abate. Approximately 50%–60% of people who experience an episode of major depressive disorder will have a second episode at some point in the future; those who have had two episodes have a 70% chance of having a third episode, and those who have had three episodes have a 90% chance of having a fourth episode (Rothschild, 1999). Although the episodes can last for months, a majority of people diagnosed with this condition (around 70%) recover within a year. However, a substantial number do not recover; around 12% show serious signs of impairment associated with major depressive disorder after 5 years (Boland & Keller, 2009). In the long-term, many who do recover will still show minor symptoms that fluctuate in their severity (Judd, 2012).
Risk Factors for Major Depressive Disorder
Major depressive disorder is a common psychiatric disorder. Around 6.6% of the US population experiences major depressive disorder each year; 16.9% will experience the disorder during their lifetime (Kessler & Wang, 2009). It is more common among women than among men, affecting approximately 20% of women and 13% of men at some point in their life (National Comorbidity Survey, 2007). The greater risk among women is not accounted for by a tendency to report symptoms or to seek help more readily, suggesting that gender differences in the rates of major depressive disorder may reflect biological and gender-related environmental experiences (Kessler, 2003).
Lifetime rates of major depressive disorder tend to be highest in North and South America, Europe, and Australia; they are considerably lower in Asian countries (Hasin, Fenton, & Weissman, 2011). The rates of major depressive disorder are higher among younger age cohorts than among older cohorts, perhaps because people in younger age cohorts are more willing to admit depression (Kessler & Wang, 2009).
A number of risk factors are associated with major depressive disorder: unemployment (including home and family caretakers); earning less than $20,000 per year; living in urban areas; or being separated, divorced, or widowed (Hasin et al., 2011). Comorbid disorders (i.e., other diseases that happen at the same time) include anxiety disorders and substance abuse disorders (Kessler & Wang, 2009).
Bipolar Disorder
A person with bipolar disorder (commonly known as manic depression) often experiences mood states that vacillate between depression and mania; that is, the person’s mood is said to alternate from one emotional extreme to the other (in contrast to unipolar, which indicates a persistently sad mood).
To be diagnosed with bipolar disorder, a person must have experienced a manic episode at least once in their life; although major depressive episodes are common in bipolar disorder, they are not required for a diagnosis (APA, 2013). According to the DSM-5, a manic episode is characterised as a “distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy lasting at least one week,” that lasts most of the time each day (APA, 2013, p. 124). During a manic episode, some experience a mood that is almost euphoric and become excessively talkative, sometimes spontaneously starting conversations with strangers; others become excessively irritable and complain or make hostile comments. The person may talk loudly and rapidly, exhibiting flights of ideas, abruptly switching from one topic to another. These individuals are easily distracted, which can make a conversation very difficult. They may exhibit grandiosity, in which they experience inflated but unjustified self-esteem and self-confidence.
For example, they might quit a job in order to “strike it rich” in the stock market, despite lacking the knowledge, experience, and capital for such an endeavour. They may take on several tasks at the same time (e.g., several time-consuming projects at work) and show little, if any, need for sleep — some may go for days without sleep. Patients may also recklessly engage in pleasurable activities that could have harmful consequences, including spending sprees, reckless driving, foolish investments, excessive gambling, or sexual encounters with strangers (APA, 2013).
During a manic episode, individuals usually feel as though they are not ill and do not need treatment. However, the reckless behaviours that often accompany these episodes — which can be antisocial, illegal, or physically threatening to others — may require involuntary hospitalization (APA, 2013). Some patients with bipolar disorder will experience a rapid-cycling subtype, which is characterised by at least four manic episodes (or some combination of at least four manic and major depressive episodes) within one year.
More About Bipolar Disorder
Watch ‘The Other Side of Me‘, in which Julie Kraft describes her lived experience with bipolar disorder.
Watch this video: The Other Side of Me – inside my bipolar mind (15 minutes)
“The Other Side of Me – inside my bipolar mind” video by Julie Kraft is licensed under the Standard YouTube Licence.
Risk Factors for Bipolar Disorder
Bipolar disorder affects people considerably less frequently than major depressive disorder. In the United States, 1 out of every 167 people meets the criteria for bipolar disorder each year, and 1 out of 100 meet the criteria within their lifetime (Merikangas et al., 2011). The rates are higher in men than in women, and about half of those with this disorder report onset before the age of 25 (Merikangas et al., 2011). Around 90% of those with bipolar disorder have a comorbid (additional) disorder, most often an anxiety disorder or a substance abuse problem. Unfortunately, close to half of the people suffering from bipolar disorder do not receive treatment (Merikangas & Tohen, 2011). Suicide rates are extremely high among those with bipolar disorder; around 36% of individuals with this disorder attempt suicide at least once in their lifetime (Novick, Swartz, & Frank, 2010), and between 15%–19% complete suicide (Newman, 2004).
The Biological Basis of Mood Disorders
Mood disorders have been shown to have a strong genetic and biological basis. Relatives of those with major depressive disorder have double the risk of developing major depressive disorder; relatives of patients with bipolar disorder have over nine times the risk (Merikangas et al., 2011). The rate of concordance (both people having the same diagnosis) for major depressive disorder is higher among identical twins (50%) than fraternal twins (38%). The pattern is similar for bipolar disorder: identical twins (67%) versus fraternal twins (16%). This suggests that genetic factors play a stronger role in bipolar disorder than in major depressive disorder (Merikangas et al. 2011).
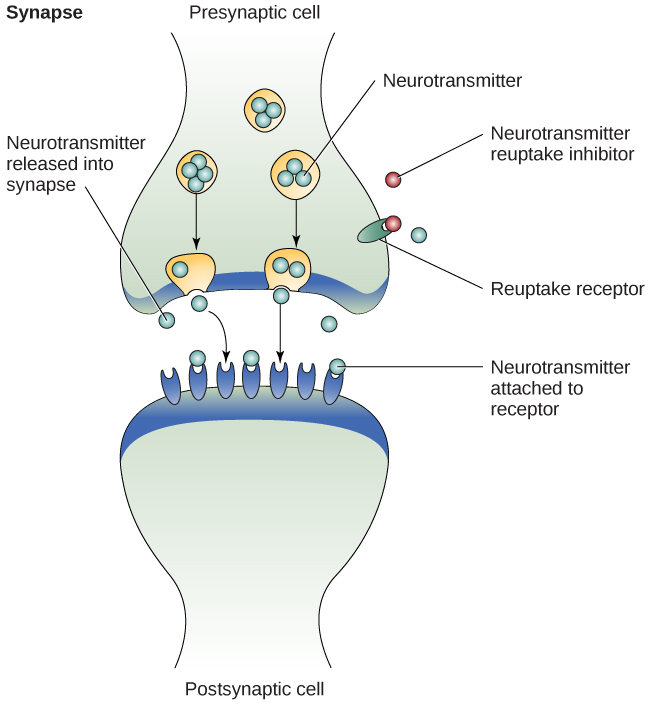
People with mood disorders often have imbalances in certain neurotransmitters, particularly norepinephrine and serotonin (Thase, 2009). These neurotransmitters are important regulators of the bodily functions that are disrupted in mood disorders, including appetite, sex drive, sleep, arousal, and mood. Medications that are used to treat major depressive disorder typically boost serotonin and norepinephrine activity, whereas lithium, which is used in the treatment of bipolar disorder, blocks norepinephrine activity at the synapses (Figure PD.13).
Cognitive Theories of Depression
Cognitive theories of depression take the view that depression is triggered by negative thoughts, interpretations, self-evaluations, and expectations (Joormann, 2009). Perhaps the most well-known cognitive theory of depression was developed in the 1960s by psychiatrist Aaron Beck, based on clinical observations and supported by research (Beck, 2008). Beck theorised that depression-prone people possess depressive schemas, or mental predispositions to think about most things in a negative way (Beck, 1976). Depressive schemas contain themes of loss, failure, rejection, worthlessness and inadequacy, and may develop early in childhood in response to adverse experiences, then remain dormant until they are activated by stressful or negative life events.
Depressive schemas prompt dysfunctional and pessimistic thoughts about the self, the world, and the future. Beck believed that this dysfunctional style of thinking is maintained by cognitive biases, or errors in how we process information about ourselves, which lead us to focus on negative aspects of experiences, interpret things negatively, and block positive memories (Beck, 2008). A person whose depressive schema consists of a theme of rejection might be overly attentive to social cues of rejection (more likely to notice another’s frown), and they might interpret this cue as a sign of rejection and automatically remember past incidents of rejection. Longitudinal studies have supported Beck’s theory in showing that a preexisting tendency to engage in this negative, self-defeating style of thinking, when combined with life stress, over time predicts the onset of depression (Dozois & Beck, 2008). Cognitive therapies for depression, aimed at changing a depressed person’s negative thinking, were developed as an expansion of this theory (Beck, 1976).

